Relationship Status: It’s complicated

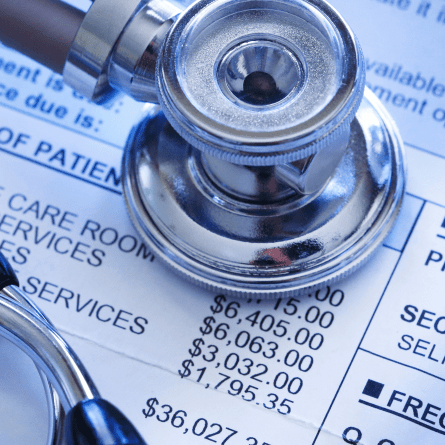
No matter who you are, in America, you have a relationship with healthcare costs. If you were born in the United States, from the moment you were born, unless your mother gave birth to you naturally with no help from a provider, you started to accrue healthcare costs. You entered this world into the hands of your service provider, or you were handed over to them. Cha-Ching. According to NHE the National Healthcare Expenditure data sheet. U.S. health care spending grew 7.5 percent in 2023, reaching $4.9 trillion or $14,570 per person. HEALTH SPENDING ACCOUNTED FOR 17.6 PERCENT OF THE NATION’S GROSS DOMESTIC PRODUCT. With so much of our spending going towards healthcare, how much do the services you receive from your providers cost? If you have medical insurance, you may know your copay, but chances are, you don’t think about the total cost of your service unless you receive a bill. It is typically only when we receive a bill from our healthcare provider that we look at how much it costs for our healthcare service and who pays what portion of it. The answer is complicated, and to answer the question, we must first understand some terms and what role they play in determining your healthcare costs.
TERMS
Health insurance
Health insurance is protection against healthcare costs you will incur. How much protection you have will depend on what type of health insurance you choose to have. The most common types of health insurance are federally funded plans like Medicare, a state and federal funded plan like Medicaid, a group insurance through your employer or an individual plan you purchase for yourself. If you don’t have protection from healthcare costs you are considered private pay, or a cash pay patient. The healthcare costs that are protected under your plan are called your benefits.
When you see a healthcare provider there are two contracts that determine your personal financial responsibility for each visit, the contract between you and your insurance and the contract between the healthcare provider and the insurance. (see visual) According to the United States Census Bureau, in 2023, 65% of covered individuals have private insurance. Private insurance is insurance provided commercially to individuals and employers.
Premium
This is the amount someone pays to have healthcare cost protection. If the person has group insurance through their employer, the employer and/or the employee may pay the premium monthly to the insurance company. An individual may pay for it if they have individual insurance coverage, or the government may pay for it for government-funded plans.
Member
A member is someone, such as a patient, who is covered by an insurance company. If you are the person paying for the insurance or it is offered by your employer, you are considered the primary member. There is a contract between the member and the insurance company regarding the monthly premiums, benefits, and the member’s financial responsibility to healthcare providers and any limitations to access to healthcare providers.
 Healthcare Provider
Healthcare Provider
A healthcare provider is a healthcare professional who provides treatment, diagnosis, therapy, and/or preventative care to members. Some examples of healthcare providers are doctors, physical therapists, and dietitians. There may or may not be a contract between the insurance company and the provider. If there is a contract, it may include negotiated fees for each service to help protect members from healthcare costs with these providers. It may also include deadlines for filing or appealing an underpaid or not paid healthcare cost.
Network Provider
These are a group of doctors from several specialties with whom insurance may have a contract. If the member’s insurance provides a network of providers, these are the preferred providers to treat their members and not utilizing these doctors could increase the member’s financial responsibility for the healthcare service. To become a network provider, a provider will fill out an application for an insurance company. The insurance company reviews the application to ensure their license is up to date, they have malpractice insurance, if the doctor is in good standing with hospitals et al and if their office fits the needs of the insurance and their members. The insurance will outline the terms of the contract such as filing deadlines, general policy and procedures for the type of healthcare provided and how much they will pay for each service. If both parties agree to the terms, the provider will become a provider in the network also known as a network provider and agrees to utilize other healthcare providers within the network for treatment of their members and to file a request for payment to the insurance company for the member.
Claim
A claim is a request for payment by the provider to the insurance company on behalf of the member. This form has a standardized format that includes the information the insurance needs to identify the patient, determine if a service is protected by the member’s benefits, and the cost it allows for each service line on the claim. They send the provider an explanation of who is financially responsible for each line item on the claim and why they are responsible for that line item. They will also send payment if they have any financial responsibility for the service. Their response is often called an explanation of benefits or explanation of payment.
Deductible
The deductible is the amount of the member’s healthcare cost that is allocated as the member’s financial responsibility before the insurance assumes any financial responsibility. This amount will vary by insurance plan. As the insurance receives claims for the member, it keeps track of how much of the financial responsibility has been allocated to the member. Once the deductible amount has been reached, the insurance will begin to accept financial responsibility for the member’s healthcare services, based on the member’s benefits. In most cases, the deductible accumulates within a calendar year. On January 1st, the amount of deductible met by a member goes back to zero and the member becomes the one financially responsible for the service.
Copay or Co-insurance
Once a member reaches their deductible, most members will have a copay or coinsurance that they are financially responsible to pay. Copays are a flat fee that you pay to your provider per visit. Co-insurance is a percentage of the contractual fee of a service that is the member’s responsibility. This amount will vary depending on the service and the contract between the provider and the insurance company.
Negotiated or allowable fee
One of the protections the insurance offers is the amount that is paid to the provider for a specific covered service if your doctor is in network with your insurance. If the doctor is in your insurance’s network, they have negotiated a contractual fee for each service. This fee is not the same for all insurance companies or providers. For example, Acme Insurance may have negotiated $75 for an office visit with Dr. A but have a different negotiated fee for Dr. B for the same service. It is the same for the providers. A provider may have negotiated one fee with Acme insurance and negotiated a different fee with Widget Insurance. However, if you receive services from a provider that is not a part of your network, there is no or little protection of your healthcare cost for that service.
And this is when your relationship with healthcare costs becomes complicated.
The basic formula for calculating the total cost of care and the member’s cost of care.
Total cost of healthcare = Insurance responsibility + Member responsibility
Member responsibility = Total cost of healthcare – Insurance responsibility
But this basic formula has many variables to consider for each portion of the equation. It must consider the member’s benefits, whether the provider was in network, if the member is the primary member on the plan and why the member needs healthcare. All this information determines how much you pay for your healthcare service and the total cost of your care.
Look for upcoming articles here that will dive deeper into each factor and how you can determine what portion is your responsibility, how to track it, and what to do if you overpaid.



Add a comment to: The Cost of Healthcare: Who pays?: Key Terms You Need to Know